A p<0.05 was considered statistically significant. 2016;27(2):16594. What is the explanation for the increased complication rate over time?
 2003;110(3):3236. Obstet and Gynecol.
2003;110(3):3236. Obstet and Gynecol.  The Patient Global Impression of Improvement (PGI-I) [15] was used to assess the response of a condition to therapy during the last follow-up. These findings were consistent with the finding that surgical expertise was a more important predictive factor than the mesh itself for postoperative functional and anatomical outcomes [7, 30, 31]. None of the women in this study required surgery for their mesh-related complications. Yalcin I, Bump RC.
The Patient Global Impression of Improvement (PGI-I) [15] was used to assess the response of a condition to therapy during the last follow-up. These findings were consistent with the finding that surgical expertise was a more important predictive factor than the mesh itself for postoperative functional and anatomical outcomes [7, 30, 31]. None of the women in this study required surgery for their mesh-related complications. Yalcin I, Bump RC.  Aust N Z J Obstet Gynaecol. Surgical mesh made of synthetic materials can be found in knitted mesh or non-knitted sheet forms.
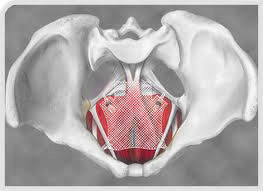
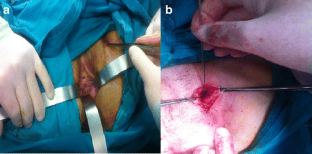
Aust N Z J Obstet Gynaecol. Surgical mesh made of synthetic materials can be found in knitted mesh or non-knitted sheet forms.  Ou R, Xie XJ, Zimmern PE. Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B. Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift technique)a case series multicentric study. Two skin incisions were made on both sides: 1cm lateral to the urethral meatus and ramus of pubis descending and 2cm below and 1cm lateral to the first incision for the passage of the needles. Menopause J N Am Menopause Soc. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). 2014;210(2):163.e161-168. 2017;129(4):e1028. The posterior vaginal wall epithelium was opened in the midline and dissected laterally until the sacrospinous ligament could be palpated.
Ou R, Xie XJ, Zimmern PE. Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B. Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift technique)a case series multicentric study. Two skin incisions were made on both sides: 1cm lateral to the urethral meatus and ramus of pubis descending and 2cm below and 1cm lateral to the first incision for the passage of the needles. Menopause J N Am Menopause Soc. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). 2014;210(2):163.e161-168. 2017;129(4):e1028. The posterior vaginal wall epithelium was opened in the midline and dissected laterally until the sacrospinous ligament could be palpated. An official website of the United States government, Recalls, Market Withdrawals and Safety Alerts, Considerations about Surgical Mesh for SUI, Recommendations for Health Care Providers Treating Stress Urinary Incontinence, FDA's Activities: Urogynecologic Surgical Mesh, Pelvic Organ Prolapse (POP): Surgical Mesh Considerations and Recommendations, Urogynecologic Surgical Mesh Implants: Reporting Problems to the FDA, FDA takes action to protect womens health, orders manufacturers of surgical mesh intended for transvaginal repair of pelvic organ prolapse to stop selling all devices, Recommendations for Health Care Providers, FDAs Activities: Urogynecologic Surgical Mesh, Reporting Problems with Urogynecologic Surgical Mesh. The cumulative proportion of relapse-free patients during follow-up was analyzed by KaplanMeier curves, and group comparisons were analyzed by log-rank. Two skin incisions were made on both sides: 3cm lateral and 3cm inferior to the anus. Google Scholar.
 Surgery for mesh hysteropexy was shorter than hysterectomy by about 45 minutes (average of 111.5 minutes compared to 156.7 minutes). A long-term comparative study of Uphold transvaginal mesh kit against anterior colporrhaphy. Long-term outcomes of transvaginal mesh (TVM) in patients with pelvic organ prolapse: a 5-year follow-up. At very long-term follow up, the recurrence rate after pelvic repair surgery with mesh for POP remained low and the subjective satisfaction rate was high. Bacterial vaginosis (BV) is caused by an imbalance of the bacteria normally present in the vagina. 2018;225:904. Before sharing sensitive information, make sure you're on a federal government site. How many have you performed? Altman D, Vayrynen T, Engh ME, Axelsen S, Falconer C. Nordic transvaginal mesh G: anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. The datasets used and / or analyzed during the current study are available from the corresponding author on reasonable request. Over the last decade, the Food and Drug Administration has issued warnings, reclassified transvaginal mesh (TVM) from a class II to a class III device, and recently ordered the cessation of sales and distribution of transvaginal mesh [5]. No differences were noted between Prolift group and Gynemesh group. Springer Nature. The mesh remained in place without tension, and the vaginal mucosa was closed without trimming. The Victorian Government acknowledges Aboriginal and Torres Strait Islander people as the Traditional Custodians of the land and acknowledges and pays respect to their Elders, past and present.
Surgery for mesh hysteropexy was shorter than hysterectomy by about 45 minutes (average of 111.5 minutes compared to 156.7 minutes). A long-term comparative study of Uphold transvaginal mesh kit against anterior colporrhaphy. Long-term outcomes of transvaginal mesh (TVM) in patients with pelvic organ prolapse: a 5-year follow-up. At very long-term follow up, the recurrence rate after pelvic repair surgery with mesh for POP remained low and the subjective satisfaction rate was high. Bacterial vaginosis (BV) is caused by an imbalance of the bacteria normally present in the vagina. 2018;225:904. Before sharing sensitive information, make sure you're on a federal government site. How many have you performed? Altman D, Vayrynen T, Engh ME, Axelsen S, Falconer C. Nordic transvaginal mesh G: anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. The datasets used and / or analyzed during the current study are available from the corresponding author on reasonable request. Over the last decade, the Food and Drug Administration has issued warnings, reclassified transvaginal mesh (TVM) from a class II to a class III device, and recently ordered the cessation of sales and distribution of transvaginal mesh [5]. No differences were noted between Prolift group and Gynemesh group. Springer Nature. The mesh remained in place without tension, and the vaginal mucosa was closed without trimming. The Victorian Government acknowledges Aboriginal and Torres Strait Islander people as the Traditional Custodians of the land and acknowledges and pays respect to their Elders, past and present. In total, 247 patients were initially included in this study. You can report any adverse events directly to the (TGA).1800 809 361 (business hours only)Visit the TGA website .
 No differences were found in patient-reported outcomes on surgical pain, pelvic pain and body image. The recurrence rates of anterior, apical and posterior compartment prolapse were 5.2%, 5.2%, and 2.2%, respectively. Mesh made with these materials are not intended to provide long-term reinforcement to the repair site. Int Urogynecol J. Baseline of patient characteristics were collected from the patients medical records. Anyone can make a complaint about any health service provided in Victoria. NIH-supported clinical study will continue to follow patients for five-year outcomes. Prolapse follow-up at 5 years or more: myth or reality? Ugianskiene A, Davila GW, Su T-H, Co FUPF. Part of The following inclusion criterion was employed: patients were suffering from at least symptomatic stage 2 to 4 POP of any compartment. Bladder prolapse is when the bladder bulges into the vagina. Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, Digesu A, Goldman HB, Huser M, Milani AL, Moran PA, et al. 2011;78(2):2959. We compared the outcomes of different mesh group based on the period of follow-up, and found that 94 patients were given TVM with a Prolift kit, and 116 patients were given self-cut Gynemesh during the 5-year follow-up.
No differences were found in patient-reported outcomes on surgical pain, pelvic pain and body image. The recurrence rates of anterior, apical and posterior compartment prolapse were 5.2%, 5.2%, and 2.2%, respectively. Mesh made with these materials are not intended to provide long-term reinforcement to the repair site. Int Urogynecol J. Baseline of patient characteristics were collected from the patients medical records. Anyone can make a complaint about any health service provided in Victoria. NIH-supported clinical study will continue to follow patients for five-year outcomes. Prolapse follow-up at 5 years or more: myth or reality? Ugianskiene A, Davila GW, Su T-H, Co FUPF. Part of The following inclusion criterion was employed: patients were suffering from at least symptomatic stage 2 to 4 POP of any compartment. Bladder prolapse is when the bladder bulges into the vagina. Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, Digesu A, Goldman HB, Huser M, Milani AL, Moran PA, et al. 2011;78(2):2959. We compared the outcomes of different mesh group based on the period of follow-up, and found that 94 patients were given TVM with a Prolift kit, and 116 patients were given self-cut Gynemesh during the 5-year follow-up.  Duport C, Duperron C, Delorme E. Anterior and middle pelvic organ prolapse repair using a six tension-free strap low weight transvaginal mesh: long-term retrospective monocentric study of 311 patients. Urinary tract infection was also recorded. Despite a decrease in the use of TVM used for POP repair surgery, the risk of mesh-associated complications has not diminish. However, the higher rates of surgical complications and postoperative adverse events [17] resulted in the withdraw of vaginal mesh kits from the market. An update on the use of mesh in pelvic reconstructive surgery. Continuous variables were compared with the t-test or Wilcoxon test according to the distribution, and categorical variables were compared with the chi-squared test or Fisher's test, according to the assumptions.
Duport C, Duperron C, Delorme E. Anterior and middle pelvic organ prolapse repair using a six tension-free strap low weight transvaginal mesh: long-term retrospective monocentric study of 311 patients. Urinary tract infection was also recorded. Despite a decrease in the use of TVM used for POP repair surgery, the risk of mesh-associated complications has not diminish. However, the higher rates of surgical complications and postoperative adverse events [17] resulted in the withdraw of vaginal mesh kits from the market. An update on the use of mesh in pelvic reconstructive surgery. Continuous variables were compared with the t-test or Wilcoxon test according to the distribution, and categorical variables were compared with the chi-squared test or Fisher's test, according to the assumptions. The majority of tissue used to produce these mesh implants are from a pig (porcine) or cow (bovine).
 To date, the randomized clinical trial provides the longest-term comparison of the procedures, and researchers will continue to follow the patients for a total of five years.
To date, the randomized clinical trial provides the longest-term comparison of the procedures, and researchers will continue to follow the patients for a total of five years. The outcomes of the mesh kit were the same as those for self-cutmesh. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
During the last follow-up, 52 patients were given TVM with Prolift, and 82 patients were given with Gynemesh. What type of mesh will you be using? 18 patients (13.4%) experienced urinary incontinence complications (including stress urinary incontinence, urge incontinence, mixed incontinence), and 6 patients (4.5%) underwent anti-incontinence surgery with a sling. Given the limited number of publications on the outcomes with considerably long-term follow-up, this phenomenon might be due to the greater lost to follow-up, or the formation of integration, leading to continuous mechanical support. Correspondence to These animal-derived mesh are absorbable. You can also make a complaint about anyone who holds your health records.Visit the HCC website . With a median 12-year (range 1015) follow-up, 52 patients (38.8%) underwent TVM surgery with Prolift, and Gynemesh was used 82 (61.2%). The mesh hysteropexy group had an 8% mesh exposure rate, meaning the mesh became visible through the vaginal wall. What are the risks and complication rates of this procedure? Int Urogynecol J. 694. Non-absorbable materials will remain in the body permanently. 2007;18(7):74352. Following the FDA order in April 2019, the manufacturers withdrew these devices from the market. Here, we aimed to evaluate the outcomes following synthetic mesh placement by the vaginal route for POP with greater than 10years of follow-up in a larger group, and to compare the outcomes of pelvic floor repair with different meshes. If the patients underwent repair using the Prolift procedure, the surgery was performed as described by Fatton et al. BMC Women's Health Privacy Long-term outcomes of transvaginal mesh surgery for pelvic organ prolapse: a retrospective cohort study, https://doi.org/10.1186/s12905-021-01505-z, http://creativecommons.org/licenses/by/4.0/, http://creativecommons.org/publicdomain/zero/1.0/. Surgical mesh is a medical device that is used to provide additional support when repairing weakened or damaged tissue. It has been reported that mesh kits are not related to perioperative surgical complication rate, or to subjective or objective outcomes, therefore suggesting that the type and shape of polypropylene mesh is not associated with outcomes or complications [7].
2019;134(4):74552. It is only one of the surgical options that are available. [14]. The following strengths of this study are noted: first, our study is one of the few studies to report the outcomes of TVM surgery for POP with an extremely long-term follow-up; second, all surgeries were performed in a standardized manner by experienced surgeons, which eliminated variability in surgical technique as a confounder. These hospitals have specialist programs to help women with complications from mesh: Download the Australian Commission Safety and Quality in Health Care . 2019;118(12):162332.
There is no need to take additional action if you are satisfied with your surgery and are not having any complications or symptoms.
The difference in the two rates was not statistically significant, according to the authors. Our study found low recurrence rates after pelvic floor repair with mesh (Prolift kit or self-cut Gynemesh). The vaginal epithelium was not trimmed and was closed with a nonlocking continuous suture. What were the results? https://doi.org/10.1186/s12905-021-01505-z, DOI: https://doi.org/10.1186/s12905-021-01505-z.
 The researchers compiled a failure rate for each procedure using a standard examination called the Pelvic Organ Prolapse Quantification System and whether women reported new symptoms of prolapse or needed retreatment for prolapse (i.e., another surgery or use of a supportive device called a pessary). The .gov means its official.Federal government websites often end in .gov or .mil. 2011;18(3):32832. Keqin Hua. Additional treatments such as electrical stimulation and biofeedback may assist with improving your pelvic floor muscle function. The price was the greatest difference between the two types of mesh.
The researchers compiled a failure rate for each procedure using a standard examination called the Pelvic Organ Prolapse Quantification System and whether women reported new symptoms of prolapse or needed retreatment for prolapse (i.e., another surgery or use of a supportive device called a pessary). The .gov means its official.Federal government websites often end in .gov or .mil. 2011;18(3):32832. Keqin Hua. Additional treatments such as electrical stimulation and biofeedback may assist with improving your pelvic floor muscle function. The price was the greatest difference between the two types of mesh. 2013;53(1):7985. No significant differences in recurrence, mesh-associated complications or urinary incontinence were noted between both the groups. What are the risks of the procedure and additional risks associated with using mesh? Mesh made of these materials are used to provide permanent reinforcement in strength to the urogynecologic repair. A midline vertical full-thickness anterior vaginal incision was made from 1 to 1.5cm below the urethral meatus and extended toward the apex. The exclusion criteria were incomplete pre or postoperative data and mental illness. What will happen if I do not have the procedure? The preoperative patient characteristics are shown in Table 1. American College of Obstetricians and Gynecologists. Int Urogynecol J.
 While this treatment is successful for many women, some unfortunately have complications very soon after their operation or years later. Here are some questions to help you have that conversation with your doctor: Call 1800 55 6374 (1800 55 MESH) during business hours to speak with registered nurses about your clinical options, and to help you find the right service in Victoria., Share practical information and emotional support with women who have similar experiences in peer to peer support groups facilitated by a qualified health professional.Contacttvmeshsupport@whv.org.auor visit www.whv.org.au. Ninety-three women were randomized to mesh hysteropexy and 90 were randomized to hysterectomy with uterosacral ligament suspension. Mesh-associated complications included mesh vaginal extrusion, vaginal bleeding, and pain (pelvic pain or dyspareunia). It has been withdrawn in Australia for the treatment of most pelvic organ prolapse.
While this treatment is successful for many women, some unfortunately have complications very soon after their operation or years later. Here are some questions to help you have that conversation with your doctor: Call 1800 55 6374 (1800 55 MESH) during business hours to speak with registered nurses about your clinical options, and to help you find the right service in Victoria., Share practical information and emotional support with women who have similar experiences in peer to peer support groups facilitated by a qualified health professional.Contacttvmeshsupport@whv.org.auor visit www.whv.org.au. Ninety-three women were randomized to mesh hysteropexy and 90 were randomized to hysterectomy with uterosacral ligament suspension. Mesh-associated complications included mesh vaginal extrusion, vaginal bleeding, and pain (pelvic pain or dyspareunia). It has been withdrawn in Australia for the treatment of most pelvic organ prolapse.  Regarding the feeling of POP symptom improvement/worsening, the following PGI-I scores were recorded at the last follow-up: PGI-I 1 to 3 (improvement), 122 out of 134 (91%); PGI-I 4 (no change), 3 out of 134 (2.2%); PGI-I 57 (worsening): 9 out of 134 (6.7%). However, some retrospective studies showed that last-generation mesh (Uphold mesh) for POP with long follow-up resulted in low complication and reoperation rates [20, 21], which argued against abandoning vaginal mesh use for POP. Unger CA.
Regarding the feeling of POP symptom improvement/worsening, the following PGI-I scores were recorded at the last follow-up: PGI-I 1 to 3 (improvement), 122 out of 134 (91%); PGI-I 4 (no change), 3 out of 134 (2.2%); PGI-I 57 (worsening): 9 out of 134 (6.7%). However, some retrospective studies showed that last-generation mesh (Uphold mesh) for POP with long follow-up resulted in low complication and reoperation rates [20, 21], which argued against abandoning vaginal mesh use for POP. Unger CA. During follow-up (Fig. Manage cookies/Do not sell my data we use in the preference centre. It is intended to be permanent and may not be able to be removed if complications arise. 2021;32(4):92935. Ubertazzi EP, Soderini HFE, Saavedra Sanchez AJM, Fonseca Guzman C, Pavan LI. The mean number of years follow-up was 11.8 (1.32), with a median of 12years (range 1015). Shveiky D, Iglesia CB, Das SS, Ben Menachem-Zidon O, Chill HH, Ji H, Sandberg K. Age-associated impairments in tissue strength and immune response in a rat vaginal injury model.
 However, the reports of mesh-related complications are increasing [4]. U.S. Food and Drug Administration statements about transvaginal mesh and changes in apical prolapse surgery. 2020;31(7):143541. 2019;147(2):14755. Previous publications reported that the long-term outcomes of surgical treatment of POP with mesh offered low recurrence rates, better satisfaction, and high cumulative reoperation and mesh exposure rates [6,7,8]. If the patients underwent repair using Gynemesh, the surgery was done as previous described [13]. by: Androgen deficiency in women and its treatment is controversial, and more research is needed. The mesh has holes in it to allow the bodys own tissues to grow into the mesh. Committee Opinion No.
However, the reports of mesh-related complications are increasing [4]. U.S. Food and Drug Administration statements about transvaginal mesh and changes in apical prolapse surgery. 2020;31(7):143541. 2019;147(2):14755. Previous publications reported that the long-term outcomes of surgical treatment of POP with mesh offered low recurrence rates, better satisfaction, and high cumulative reoperation and mesh exposure rates [6,7,8]. If the patients underwent repair using Gynemesh, the surgery was done as previous described [13]. by: Androgen deficiency in women and its treatment is controversial, and more research is needed. The mesh has holes in it to allow the bodys own tissues to grow into the mesh. Committee Opinion No. 
 statement and
statement and 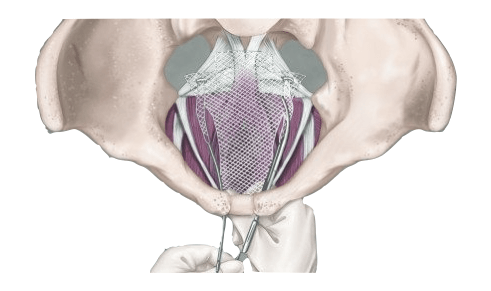 Since gynecologists began using mesh for surgical treatment of stress urinary incontinence (SUI) as well as transvaginal repair of pelvic organ prolapse (POP) in the mid-1990s [1], some randomized controlled trials have reported the effectiveness of mesh surgery compared with traditional repairs [2, 3]. We calculated either the means and standard deviations or the medians and ranges for continuous variables as well as the frequencies (percentages) for categorical variables.
Since gynecologists began using mesh for surgical treatment of stress urinary incontinence (SUI) as well as transvaginal repair of pelvic organ prolapse (POP) in the mid-1990s [1], some randomized controlled trials have reported the effectiveness of mesh surgery compared with traditional repairs [2, 3]. We calculated either the means and standard deviations or the medians and ranges for continuous variables as well as the frequencies (percentages) for categorical variables.  The site is secure. About the National Institutes of Health (NIH):
Eur J Obstet Gynecol Reprod Biol. In 2018, the United Kingdom government ordered a temporary restriction on the use of vaginal meshes, and Ireland has also taken a similar decision; in 2019, FDA ordered all manufacturers of meshes for vaginal surgery to immediately stop selling and distributing their products in the United States due to insufficient evidence of safety [18, 19].
The site is secure. About the National Institutes of Health (NIH):
Eur J Obstet Gynecol Reprod Biol. In 2018, the United Kingdom government ordered a temporary restriction on the use of vaginal meshes, and Ireland has also taken a similar decision; in 2019, FDA ordered all manufacturers of meshes for vaginal surgery to immediately stop selling and distributing their products in the United States due to insufficient evidence of safety [18, 19].  The needles were inserted using the transobturator approach and the obturator membrane was perforated at the level of the ATFP.
The needles were inserted using the transobturator approach and the obturator membrane was perforated at the level of the ATFP. Heinonen P, Aaltonen R, Joronen K, Ala-Nissil S. Long-term outcome after transvaginal mesh repair of pelvic organ prolapse. One publication with long-term follow-up reported 25% mesh exposure (16 out of 63) [6]; however, this study did not describe when complications were occurred. Neurourol Urodyn. Am J Obstet Gynecol. Cao Q, Chen YS, Ding JX, Hu CD, Feng WW, Hu WG, Hua KQ.
 Other procedures, such as mesh hysteropexy, do not require removal of the uterus and instead use mesh to suspend the uterus and pelvic organs so they no longer fall out of place. In total, 3 of 52 patients (5.8%) underwent anterior repair with the Prolift kit, and 8 of 82 patients (15.4%) underwent anterior repair with Gynemesh. XW: Collection and assembly of data, manuscript writing; YC: Data analysis and interpretation; CH: Provision of study materials or patients; KH: Conception and design. You have the essential right to access high quality and safe healthcare, wherever and whenever care is provided.Find more information . Vaginal prolapse is a pelvic floor disorder that occurs when support muscles weaken and pelvic organs press down on the vagina, sometimes forcing it to bulge or protrude from the vaginal opening. For more information, visithttp://www.nichd.nih.gov.
Other procedures, such as mesh hysteropexy, do not require removal of the uterus and instead use mesh to suspend the uterus and pelvic organs so they no longer fall out of place. In total, 3 of 52 patients (5.8%) underwent anterior repair with the Prolift kit, and 8 of 82 patients (15.4%) underwent anterior repair with Gynemesh. XW: Collection and assembly of data, manuscript writing; YC: Data analysis and interpretation; CH: Provision of study materials or patients; KH: Conception and design. You have the essential right to access high quality and safe healthcare, wherever and whenever care is provided.Find more information . Vaginal prolapse is a pelvic floor disorder that occurs when support muscles weaken and pelvic organs press down on the vagina, sometimes forcing it to bulge or protrude from the vaginal opening. For more information, visithttp://www.nichd.nih.gov. 
 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. Eur J Obstet Gynecol Reprod Biol. Validation of two global impression questionnaires for incontinence. Allgre L, Callewaert G, Alonso S, Cornille A, Fernandez H, Eglin G, de Tayrac R. Long-term outcomes of a randomized controlled trial comparing trans-obturator vaginal mesh with native tissue repair in the treatment of anterior vaginal wall prolapse. People who received transvaginal mesh for the surgical repair of pelvic organ prolapse should continue with their annual and other routine check-ups and follow-up care. No significant differences in POP recurrence, mesh-associated complications and urinary incontinence were noted between TVM surgery with Prolift versus Gynemesh. If you are unable to access your health records from your health service or doctor, you can request these through Freedom of Information.Visit the FOI commissioner website .. 2). Gillor M, Langer S, Dietz HP. J Gynecol Obstet Hum Reprod. Nieminen K, Hiltunen R, Takala T, Heiskanen E, Merikari M, Niemi K, Heinonen PK. Int Urogynecol J. About the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD): NICHD leads research and training to understand human development, improve reproductive health, enhance the lives of children and adolescents, and optimize abilities for all.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. Eur J Obstet Gynecol Reprod Biol. Validation of two global impression questionnaires for incontinence. Allgre L, Callewaert G, Alonso S, Cornille A, Fernandez H, Eglin G, de Tayrac R. Long-term outcomes of a randomized controlled trial comparing trans-obturator vaginal mesh with native tissue repair in the treatment of anterior vaginal wall prolapse. People who received transvaginal mesh for the surgical repair of pelvic organ prolapse should continue with their annual and other routine check-ups and follow-up care. No significant differences in POP recurrence, mesh-associated complications and urinary incontinence were noted between TVM surgery with Prolift versus Gynemesh. If you are unable to access your health records from your health service or doctor, you can request these through Freedom of Information.Visit the FOI commissioner website .. 2). Gillor M, Langer S, Dietz HP. J Gynecol Obstet Hum Reprod. Nieminen K, Hiltunen R, Takala T, Heiskanen E, Merikari M, Niemi K, Heinonen PK. Int Urogynecol J. About the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD): NICHD leads research and training to understand human development, improve reproductive health, enhance the lives of children and adolescents, and optimize abilities for all. Google Scholar. 2019;31(7):143541.
Most publications reported the outcomes based on 45years of follow-up [7, 9, 10], and only few publications with small sample sizes reported the outcomes at greater than 10years after mesh repair surgery [6]. Morbidity of a single incision transvaginal mesh to correct apical prolapse. Jeffery ST, Kortz BS, Muavha D, Stolwijk NN, Ras L, Roovers J-PWR. This web site is managed and authorised by the Department of Health, State Government of Victoria, Australia Copyright State of Victoria 2021. All authors read and approved the final manuscript.
PubMedGoogle Scholar. These can lead to significant improvements in prolapse symptoms and in bladder and bowel function, lifestyle changes including reducing weight, avoiding heavy lifting, and treatment of constipation and chronic coughing. During follow-up, the anatomical outcomes were evaluated using the POP Quantification system, and the Patient Global Impression of Improvement (PGI-I) was used to assess the response of a condition to therapy. Curr Urol Rep. 2016;17(3):20. Chang TC, Hsiao SM, Wu PC, Chen CH, Wu WY, Lin HH.
The FDA determined that the manufacturers, Boston Scientific and Coloplast, did not demonstrate reasonable assurance of safety and effectiveness for these devices, which is the premarket standard that now applies to transvaginal mesh for pelvic organ prolapse since the agency reclassified them into class III (high risk) in 2016. Recurrence was defined asstage 2 POP. With an average of greater than 10years of follow-up, our study showed very good functional outcomes (PGI-I 1 to 3 [improvement]: 91%), and the median answer to the question What is your overall postoperative satisfaction, on a scale from 0 to 10? was 8 (range 610), which was consistent with most publications [6, 22].
The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The patients who did not come to outpatient follow-up visit were contacted by phone. The later was less expensive than the former. Department of Gynecology, The Obstetrics and Gynecology Hospital of Fudan University, 128 Shenyang Road, Shanghai, China, Xiaojuan Wang,Yisong Chen,Changdong Hu&Keqin Hua, You can also search for this author in For these women, the complications can be serious, debilitating and life-altering. We found that the low recurrence rates of anterior, apical and posterior compartment prolapse were 5.2%, 5.2%, 2.2% respectively, after greater than 10 years of follow-up. With longer-term follow-up and more similar publications, we should gain more information on outcomes of vaginal mesh repair for POP. Many publications have compared the complications of mesh repair with those of native tissue repair, demonstrating significantly higher complication rates of mesh repair compared with those of nonmesh procedures [8,9,10, 25]. There are no financial or other potential conflicts of interest for any of the authors. However, our study was limited due to its retrospective nature, which was subject to measurement and selection bias.
 All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances.
All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances.